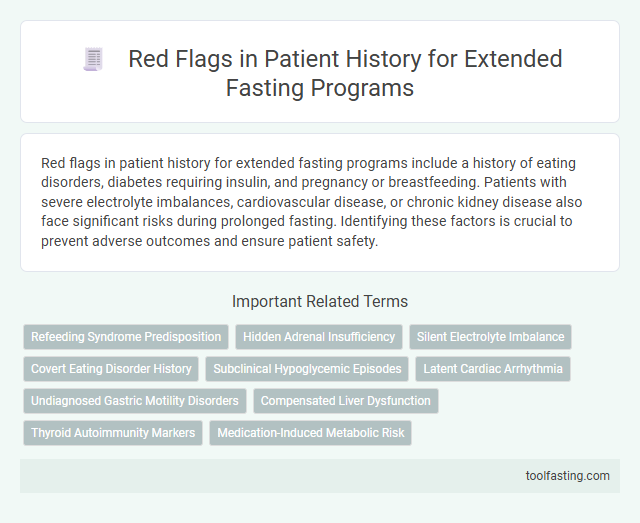
Red flags in patient history for extended fasting programs include a history of eating disorders, diabetes requiring insulin, and pregnancy or breastfeeding. Patients with severe electrolyte imbalances, cardiovascular disease, or chronic kidney disease also face significant risks during prolonged fasting. Identifying these factors is crucial to prevent adverse outcomes and ensure patient safety.
Introduction: Importance of Patient Screening for Extended Fasting
Extended fasting offers numerous health benefits but carries significant risks if not properly supervised. Careful patient screening is crucial to identify potential dangers and ensure safe fasting practices.
- Pre-existing medical conditions - Chronic illnesses such as diabetes or cardiovascular disease can increase fasting risks and require thorough evaluation.
- Medication use - Certain medications impact metabolism and hydration status, necessitating close monitoring during extended fasting.
- History of eating disorders - Prior or active eating disorders elevate the risk of adverse psychological and physiological effects during fasting.
Effective risk assessment and patient history review are foundational steps for safe and beneficial extended fasting programs.
History of Eating Disorders
History of eating disorders poses significant risks for patients considering extended fasting programs. These disorders can lead to severe physiological and psychological complications during fasting.
Patients with a history of anorexia nervosa, bulimia, or binge-eating disorder should undergo thorough evaluation before fasting. Close monitoring is essential to prevent relapse and ensure patient safety.
Diagnosed Metabolic or Endocrine Disorders
Patients with diagnosed metabolic or endocrine disorders require careful evaluation before beginning extended fasting programs. Conditions such as diabetes, thyroid dysfunction, and adrenal insufficiency can significantly impact the safety and efficacy of prolonged fasting. Identifying these red flags in patient history is crucial to prevent adverse events and tailor fasting protocols appropriately.
Use of Glucose-Lowering Medications
Does the patient use glucose-lowering medications? Glucose-lowering drugs can increase the risk of hypoglycemia during extended fasting, requiring close monitoring and possible medication adjustments.
Reports of Cardiovascular Disease
| Red Flag | Description | Implications for Extended Fasting |
|---|---|---|
| History of Myocardial Infarction (Heart Attack) | Previous heart attack indicates compromised cardiac function and increased vulnerability. | Extended fasting may exacerbate cardiac stress; requires close medical supervision and possible contraindication. |
| Unstable Angina | Episodes of chest pain due to inadequate blood flow to the heart, signaling unstable cardiovascular status. | High risk for adverse events during extended fasting; fasting likely contraindicated until stabilization. |
| Congestive Heart Failure (CHF) | Condition where the heart's ability to pump blood is impaired, leading to fluid retention and fatigue. | Fasting may worsen fluid imbalance and cardiac workload; extended fasts generally not recommended. |
| Arrhythmias or Irregular Heartbeats | Abnormal heart rhythms, such as atrial fibrillation or ventricular tachycardia, which can compromise cardiac output. | Risk of complications increased with electrolyte imbalances from fasting; careful monitoring required if fasting proceeds. |
| History of Stroke or Transient Ischemic Attack (TIA) | Previous cerebrovascular events indicating underlying vascular disease and risk of recurrence. | Fasting must be approached with caution due to potential impacts on blood pressure and clotting factors. |
| Peripheral Artery Disease | Narrowing of peripheral arteries reducing blood flow, often coexisting with cardiovascular disease. | Extended fasting may affect vascular health and circulation; clinical evaluation advised before fasting. |
| Use of Cardiovascular Medications (e.g., Beta-Blockers, Anticoagulants) | Medications may influence heart rate, blood pressure, and coagulation status during fasting periods. | Potential drug-nutrient interactions and risk of adverse effects necessitate close monitoring and medical consultation. |
| Elevated Blood Pressure or History of Hypertension | Chronic high blood pressure increases cardiovascular risk and affects fasting tolerance. | Blood pressure should be well-controlled prior to extended fasting; monitoring essential during fasting. |
History of Electrolyte Imbalances
History of electrolyte imbalances presents a significant red flag for extended fasting programs. Patients with previous episodes of hypokalemia, hyponatremia, or hyperkalemia require careful assessment before initiating prolonged fasting.
Electrolyte disturbances can lead to severe cardiac arrhythmias, muscle weakness, and neurological symptoms during fasting. Continuous monitoring of serum electrolytes is essential to mitigate risks and ensure patient safety throughout the fasting period.
Chronic Kidney or Liver Disease
Extended fasting programs require careful screening to identify patients with potential risks due to chronic kidney or liver disease. Such conditions can significantly impact the safety and efficacy of prolonged fasting protocols.
- Impaired Renal Function - Chronic kidney disease reduces the body's ability to filter waste, increasing the risk of toxin buildup during fasting.
- Hepatic Dysfunction - Liver disease impairs metabolism and nutrient storage, potentially leading to severe hypoglycemia or electrolyte imbalances.
- Altered Drug Clearance - Both kidney and liver diseases can affect medication metabolism, causing toxic accumulation during fasting periods.
Previous Episodes of Syncope or Severe Dizziness
Previous episodes of syncope or severe dizziness present significant red flags in patient history for extended fasting programs. These symptoms may indicate underlying cardiovascular or neurological issues that can be exacerbated by prolonged fasting. Your safety depends on thorough evaluation before beginning any extended fasting regimen to prevent serious complications.
Active or Recent Pregnancy and Breastfeeding
Active or recent pregnancy is a critical red flag in extended fasting programs due to increased nutritional needs that support fetal development and maternal health. Breastfeeding similarly requires adequate nutrition to ensure sufficient milk production and infant growth.
You must avoid extended fasting if you are currently pregnant or breastfeeding, as it can lead to nutrient deficiencies and harm both you and your baby. Hormonal changes and energy demands during these periods increase the risk of adverse effects from prolonged fasting. Proper medical evaluation is essential before considering any fasting regimen in these conditions.
Related Important Terms
Refeeding Syndrome Predisposition
Patients with a history of malnutrition, chronic alcoholism, prolonged fasting, electrolyte imbalances, or conditions such as anorexia nervosa and severe weight loss are at a high risk of developing refeeding syndrome during extended fasting programs and require careful monitoring of phosphate, potassium, and magnesium levels to prevent life-threatening complications.
Hidden Adrenal Insufficiency
Hidden adrenal insufficiency, often undiagnosed in patients undergoing extended fasting programs, poses significant risks such as severe fatigue, hypotension, electrolyte imbalances, and impaired stress response, necessitating thorough screening through cortisol level assessments and patient history evaluation to prevent adrenal crisis and support safe fasting practices.
Silent Electrolyte Imbalance
Silent electrolyte imbalance presents a critical red flag in patient history for extended fasting programs as it can lead to life-threatening complications such as cardiac arrhythmias, muscle weakness, and neurological disturbances, necessitating thorough pre-fasting assessments including serum electrolyte panels and continuous monitoring to mitigate risks.
Covert Eating Disorder History
A covert eating disorder history in patient records represents a significant red flag for extended fasting programs, as underlying disordered eating behaviors such as anorexia nervosa, bulimia nervosa, or binge eating disorder can increase risks of malnutrition, electrolyte imbalances, and psychological distress during prolonged fasting periods.
Subclinical Hypoglycemic Episodes
Subclinical hypoglycemic episodes in patient history signal a critical red flag for extended fasting programs due to the increased risk of unnoticed blood glucose drops leading to severe metabolic complications and compromised patient safety, emphasizing the need for continuous glucose monitoring and thorough pre-fasting assessment to mitigate potential adverse events.
Latent Cardiac Arrhythmia
Latent cardiac arrhythmia, often undiagnosed in routine exams, represents a critical red flag in patient history for extended fasting programs due to its potential to precipitate life-threatening irregular heart rhythms during prolonged caloric restriction, emphasizing the necessity for comprehensive cardiac monitoring and pre-fast screening such as Holter monitoring or electrocardiogram (ECG) evaluations to mitigate risks associated with electrolyte imbalances and autonomic nervous system fluctuations inherent in extended fasting protocols.
Undiagnosed Gastric Motility Disorders
Undiagnosed gastric motility disorders, such as gastroparesis or chronic intestinal pseudo-obstruction, present significant red flags in patient history for extended fasting programs due to their potential to impair gastric emptying, exacerbate gastrointestinal symptoms, and increase the risk of severe complications like malnutrition, bezoar formation, and electrolyte imbalances, necessitating thorough diagnostic evaluation before initiating prolonged fasting protocols.
Compensated Liver Dysfunction
Compensated liver dysfunction in patient history serves as a critical red flag for extended fasting programs due to impaired hepatic metabolism, altered glycogen storage, and increased risk of hepatic decompensation, necessitating thorough liver function assessment and close monitoring for signs of encephalopathy, coagulopathy, or ascites during fasting interventions.
Thyroid Autoimmunity Markers
Elevated thyroid autoimmunity markers such as anti-thyroid peroxidase (anti-TPO) and anti-thyroglobulin antibodies indicate a significant risk factor in patient history for extended fasting programs, as these markers correlate with autoimmune thyroid conditions that may exacerbate during prolonged caloric restriction, necessitating careful monitoring and individualized risk assessment to prevent potential hypothyroid complications.
Red Flags in Patient History for Extended Fasting Programs Infographic