Semantic risk factors in extended fasting protocols involve identifying and evaluating behavioral, physiological, and environmental conditions that may compromise safety and effectiveness. These factors include underlying health conditions such as diabetes or cardiovascular issues, medication interactions, and signs of nutrient deficiencies or electrolyte imbalances. Accurate assessment of these risks ensures personalized fasting plans that minimize adverse effects and support optimal metabolic outcomes.
Understanding Semantic Risk in Fasting Protocols
Understanding semantic risk in fasting protocols involves recognizing the nuanced factors that influence safety and effectiveness. Extended fasting carries unique challenges that require careful evaluation of individual health conditions and lifestyle variables.
Semantic risk factors include medical history, metabolic responses, and psychological readiness, which all affect fasting outcomes. Identifying these elements helps anticipate potential complications and tailor fasting plans accordingly. You must approach extended fasting with informed awareness to minimize adverse effects and maximize benefits.
Defining Extended Fasting and Its Scope
Extended fasting refers to abstaining from caloric intake for a period longer than 24 hours, typically ranging from 48 to 72 hours or more. This practice aims to induce metabolic shifts such as ketosis and autophagy, impacting cellular repair and energy utilization. Defining the scope of extended fasting involves understanding both the physiological effects and the potential risks associated with prolonged fasting periods.
Misinterpretation of Fasting Outcomes
| Semantic Risk Factor | Description | Impact on Extended Fasting |
|---|---|---|
| Misinterpretation of Fasting Outcomes | Incorrect understanding or evaluation of physiological responses during fasting periods, such as weight fluctuations, ketone levels, or energy changes. | Leads to premature discontinuation, unsafe fasting extension, or failure to recognize harmful symptoms, increasing the risk of adverse health effects. |
Ambiguity in Terminology and Protocol Guidelines
Ambiguity in terminology and protocol guidelines significantly impacts the effectiveness of Extended Fasting Risk Assessment Tools. Inconsistent definitions of fasting duration, dietary intake, and refeeding stages create challenges in standardizing risk evaluations. Clear, precise language in fasting protocols enhances accuracy in identifying potential adverse effects and improves patient safety during extended fasting regimens.
Risks of Generalization Across Populations
Extended fasting protocols often fail to account for the diverse physiological and metabolic differences across various populations. Generalizing risk assessments without population-specific data can lead to inaccurate evaluations of potential health complications.
Factors such as age, genetics, pre-existing medical conditions, and lifestyle behaviors heavily influence fasting tolerance and outcomes. Ignoring these variables increases the risk of adverse events and undermines the safety and efficacy of fasting regimens.
Inconsistent Communication Among Practitioners
Inconsistent communication among practitioners during extended fasting protocols can lead to critical gaps in patient monitoring and care coordination. This risk factor amplifies the potential for adverse events by compromising the clarity and continuity of medical instructions and updates.
- Fragmented Information Exchange - Lack of standardized communication methods causes incomplete sharing of patient data and fasting progress among healthcare providers.
- Conflicting Guidance - Diverse professional opinions without cohesive discussion result in contradictory advice that may confuse patients and impair compliance.
- Delayed Response to Complications - Inefficient communication channels slow the identification and management of fasting-related side effects, increasing health risks for patients.
Patient Misunderstanding Due to Vague Instructions
Extended fasting protocols require clear communication to ensure patient safety and efficacy. Misunderstandings from vague instructions can lead to serious health risks and non-compliance.
- Ambiguous Guidelines - Patients often misinterpret unclear fasting duration or permissible intake, resulting in inconsistent adherence.
- Inadequate Explanation of Symptoms - Lack of detailed symptom information may cause patients to ignore warning signs of adverse effects during fasting.
- Insufficient Follow-up Instructions - Patients may be uncertain about post-fast refeeding protocols, increasing the risk of digestive complications.
Clear, detailed instructions are essential to minimize semantic risks and enhance patient outcomes in extended fasting.
Overlooking Individual Health Variance
Have you considered how your unique health conditions impact extended fasting safety? Overlooking individual health variance can lead to unpredictable risks during an extended fasting protocol. Personal medical history and current health status are critical factors that influence fasting outcomes.
Semantic Barriers in Research and Data Reporting
Semantic barriers in extended fasting research limit clear communication and data accuracy, affecting the reliability of fasting protocol assessments. These barriers create challenges in interpreting results and forming comprehensive risk profiles for extended fasting practices.
- Inconsistent Terminology - Varying definitions of 'fasting' and 'extended fasting' lead to confusion in data comparison across studies.
- Ambiguous Reporting Standards - Lack of standardized frameworks for symptom and outcome reporting hinders uniform risk evaluation.
- Data Fragmentation - Disparate data sources and classification methods cause incomplete aggregation of safety and efficacy information, impacting Your risk assessment accuracy.
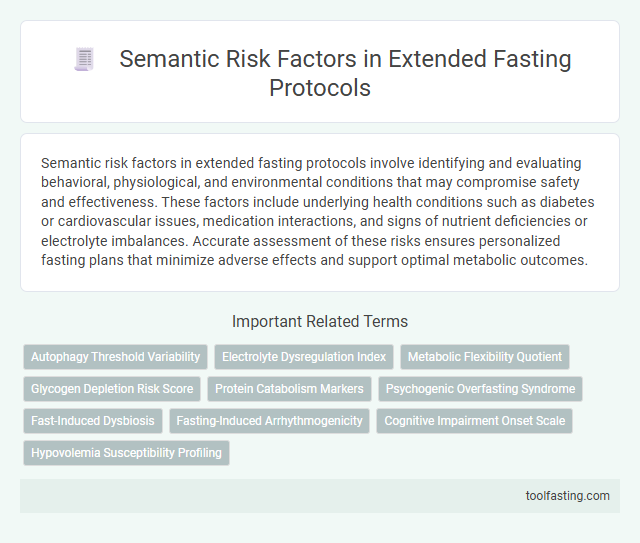
Related Important Terms
Autophagy Threshold Variability
Autophagy threshold variability significantly influences individual responses to extended fasting protocols by affecting the onset and intensity of cellular recycling processes, which necessitates personalized risk assessment to optimize fasting duration and minimize adverse effects such as excessive catabolism or nutrient deficiencies.
Electrolyte Dysregulation Index
Electrolyte Dysregulation Index in extended fasting protocols quantifies the risk of imbalances in critical electrolytes such as sodium, potassium, magnesium, and calcium, which are essential for maintaining cellular function, nerve transmission, and cardiac stability during prolonged periods without food intake.
Metabolic Flexibility Quotient
Metabolic Flexibility Quotient, a critical metric in extended fasting risk assessment tools, evaluates the body's ability to efficiently switch between carbohydrate and fat metabolism, directly influencing the risk of hypoglycemia and insulin resistance during prolonged fasting periods; lower metabolic flexibility indicates higher susceptibility to energy imbalance, increased oxidative stress, and potential metabolic derangements, making it essential for clinicians to incorporate this quotient when personalizing extended fasting protocols to optimize safety and efficacy.
Glycogen Depletion Risk Score
Glycogen Depletion Risk Score quantifies the likelihood of adverse effects during extended fasting by evaluating factors such as baseline muscle mass, liver glycogen reserves, physical activity levels, metabolic rate, and nutritional status to optimize fasting protocols and mitigate hypoglycemia and muscle catabolism.
Protein Catabolism Markers
Protein catabolism markers such as elevated blood urea nitrogen (BUN), increased creatinine levels, and high plasma ammonia are critical semantic risk factors indicating muscle breakdown and impaired nitrogen balance during extended fasting protocols, necessitating careful monitoring to prevent muscle wasting and metabolic complications.
Psychogenic Overfasting Syndrome
Psychogenic Overfasting Syndrome, characterized by compulsive fasting behavior driven by psychological factors such as anxiety, depression, or obsessive-compulsive tendencies, represents a critical semantic risk factor in extended fasting protocols due to its potential to exacerbate malnutrition, electrolyte imbalances, and psychological distress, thereby necessitating comprehensive mental health screening and continuous psychological support within the Extended Fasting Risk Assessment Tool to prevent adverse outcomes.
Fast-Induced Dysbiosis
Fast-induced dysbiosis, characterized by significant alterations in gut microbiota diversity and function during extended fasting protocols, poses critical risks including impaired immune response, increased gut permeability, and metabolic disturbances, necessitating precise assessment of microbial shifts, host-microbe interactions, and inflammatory biomarkers to optimize safety and efficacy in prolonged fasting interventions.
Fasting-Induced Arrhythmogenicity
Fasting-induced arrhythmogenicity represents a critical semantic risk factor in extended fasting protocols, characterized by alterations in electrolyte balance, increased sympathetic activity, and prolonged QT intervals that collectively elevate the potential for cardiac arrhythmias and sudden cardiac events, necessitating thorough pre-fasting cardiovascular evaluation and continuous monitoring during prolonged fasts to mitigate adverse outcomes.
Cognitive Impairment Onset Scale
The Cognitive Impairment Onset Scale within the Extended Fasting Risk Assessment Tool quantifies risk levels by evaluating biomarkers such as blood glucose variability, ketone body concentrations, and neuroinflammatory markers to predict early cognitive decline during prolonged fasting protocols.
Semantic Risk Factors in Extended Fasting Protocols Infographic